Health Conditions
What is Coronary Artery Disease?
Coronary artery disease (CAD), also called coronary heart disease or heart disease, is responsible for approximately one third of all deaths in people over 35 worldwide.1 CAD results from arteriosclerosis, a narrowing of the blood vessel. In some cases, coronary artery disease can totally block the supply of oxygen-rich blood to the heart muscle, causing a heart attack.
What causes CAD?
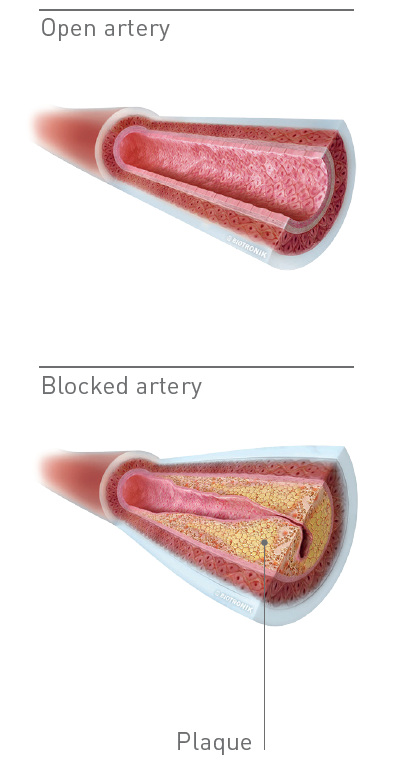
CAD is the narrowing (or stenosis) of the arteries in the heart. Coronary arteries are blood vessels that play a vital role in keeping your heart healthy by carrying oxygen to the heart muscle. Although arteries are normally smooth on the inside, they can become narrowed or blocked by a buildup of fat or calcium deposits on the artery wall, called plaques. As more plaque builds up, your arteries narrow and stiffen through a process called atherosclerosis (a sort of hardening of the arteries).
When this hardening occurs, blood flow can be reduced, and your heart may not receive the oxygen it needs.
The lack of blood flow can result in chest pain (angina pectoris) and shortness of breath (dyspnea) during exercise, emotional stress or even at rest. As the plaque grows, it can completely block the artery, preventing part of the heart muscle from receiving oxygen and causing a heart attack, also called myocardial infarction. Vessels are often blocked or narrowed in multiple spots. A myocardial infarction is often caused by the rupture of a plaque, meaning some of the fatty build up becomes loose in the bloodstream.
When fat or calcium deposits are loose in the bloodstream they can become lodged in the artery, blocking the flow of blood. In a myocardial infarction patients often suffer from severe chest pain (angina pectoris) and shortness of breath (dyspnea). The patients often start sweating and can be in a great deal of pain.
What are the risk factors for CAD?
There are a number of risk factors for CAD, and the more risk factors you have, the greater the chance of developing it. However, the good news is that for most of these risk factors, you can do something about them.
- Age (over 45 for men, over 55 for women)
- Family history of heart and vascular disease
- Diabetes
- Smoking
- High blood pressure
- High levels of LDL cholesterol and triglycerides
- Low levels of HDL cholesterol
- Being overweight or obese
- Sedentary lifestyle
- Emotional stress
How do I recognize CAD?
Because arteries narrow and harden gradually over the years, it can take decades before patients experience discomfort. The first symptoms usually appear when the heart is under stress – for example, during exercise. Symptoms vary and may also occur at rest or during sleep.
If you suspect you are having a heart attack or are experiencing chest discomfort, especially with the following symptoms, seek medical help immediately:
- Discomfort, pressure or pain in the center of the chest or radiating to one or both arms or jaw
- Pain in the neck, jaw, throat, abdomen or back
- Shortness of breath
- Fast heart beat or heart palpitations
- Dizziness or sweating
- Nausea or vomiting
- Quick exhaustion during physical activity which did not use to cause symptoms
If you have these symptoms, even rarely or temporarily, consult your physician.
Men over 45 years and women over 55 should have regular checkups.
How is CAD diagnosed?
A number of different tests may be used to diagnose CAD. If you feel anxious about having a test, ask your partner, friend or relative to come along to the appointment with you.
- Electrocardiography (ECG or EKG): Records the electrical activity of your heart. It can show typical signs for a lack of myocardial oxygen-supply (myocardial ischemia)
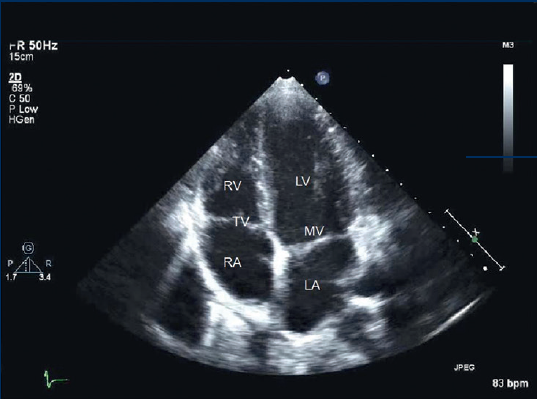
- Echocardiogram (ECHO): Uses ultrasound (high-frequency sound waves) to give accurate information about the structure and pumping action of your heart
- Treadmill-test: Before, during or after exercise an ECG is recorded and blood-pressure is evaluated. The physician checks the ECGs for signs of myocardial ischemia
- Stress-echo: Sometimes an ECHO is done while the heart is put under stress by increasing its heart rate – either with exercise or with a certain type of medicine. If parts of the heart muscle are damaged, they will contract less effectively, and this can show up on the ECHO
- Computerized tomography (CT): A type of X-ray scan used to show the calcification of the coronary arteries and the blood flow through them. It is very sensitive for the detection of any narrowing
- Magnetic resonance imaging (MRI): A non-invasive method which produces extremely detailed pictures of the heart to identify damaged areas (called lesions) in the arteries
- Blood tests: A series of tests that can help diagnose heart problems. For example, the troponin test is used to find out if your heart muscle is damaged
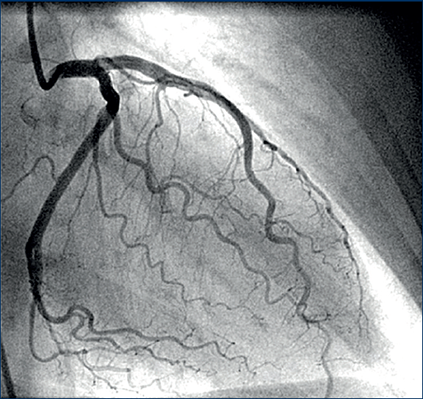
- Catheterization of the heart (also called coronary angiography): A test done in a catheterization laboratory (‘cath lab’) in which a cardiologist injects a special dye (called a contrast dye). X-ray images of the heart then show where the coronary vessels are narrowed and how severe the narrowing is. This test is essential for deciding what sort of treatment you should be offered
- Intracoronary flow reserve (iFR): With a special wire the cardiologist can evaluate the significance of a stenosis by measuring the blood pressure previous and after a stenosis
- Intravascular ultrasound (IVUS): Performed in the cath lab using high-frequency ultrasound waves to look inside the artery
An ECHO image of the heart
A coronary angiogram lets doctors watch the activity inside the heart
1 Wilson PWF and Douglas PS. Epidemiology of coronary heart disease. 2015. UpToDate- Wolters Kluwer Health.http://www.uptodate.com/contents/epidemiology-of-coronary-heart-disease

