Overview
Why would your patients need a comprehensive physiologic sensor, like CLS?
Every person experiences physical and emotional stress during their life. Regular daily activities, sport, or even playing chess or watching a video can result in such stress. If they suffer from chronotropic incompetence (CI), the patient's heart is not able to respond correctly to the stimulus. Studies have shown that CLS can improve the quality of life of CI patients as well as those suffering from vasovagal syncope.¹
Thanks to CLS rate adaptation, pacemaker patients are also supported during emotional stress.
Which patients can benefit from CLS?
CLS is beneficial for patients with Chronotropic Incompetence (CI) and Vasovagal Syncope (VS) as well as patients with Atrial Fibrillation (AF). For patients suffering from CI, the PROVIDE study showed that 75% of patients programmed with DDD-CLS experienced significant improvement compared to only 22% of patients programmed in DDDR.²
For patients suffering from VS, the recurrence of syncope significantly decreases with a CLS system. The randomized, placebo-controlled, double-blinded, multicenter BIOSync CLS study demonstrated a reduction of syncope recurrence rate after two years by 77% with CLS pacing versus placebo³.
For patients burdened with paroxysmal or permanent atrial fibrillation (AF), cardiac output is also of utmost importance when AV synchrony is lost. CLS is able to support these patients through a steady, reliable and flexible algorithm. CLS has also been shown to reduce the burden for atrial tachycardia patients compared with other modes. The BURDEN study I demonstrated that patients with CLS sensor had on average 0.11 min/day of AT burden while with DDDR mode patients had on average 10.9 min/day of AT burden.⁴ Subsequently, the BURDEN Study II equally showed a lower AT burden with the CLS sensor. ⁵
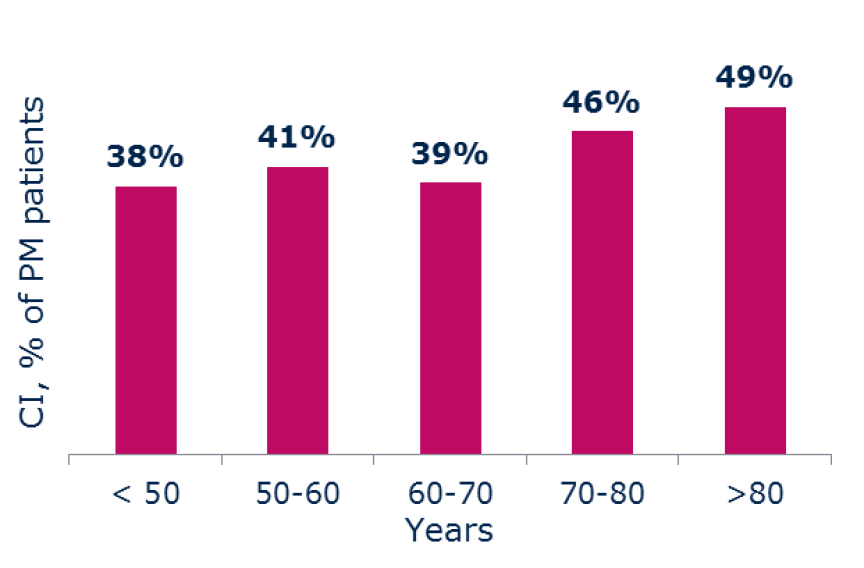
About 40% of your pacemaker patients between 70 and 80 years old suffer from chronotropic incompetence.⁶ The CLS sensor could help these patients to get back an emotional life!
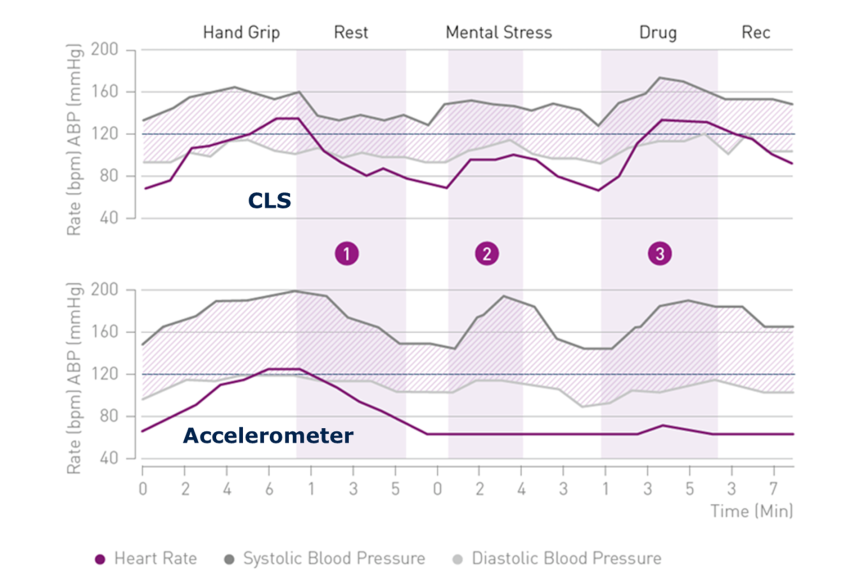
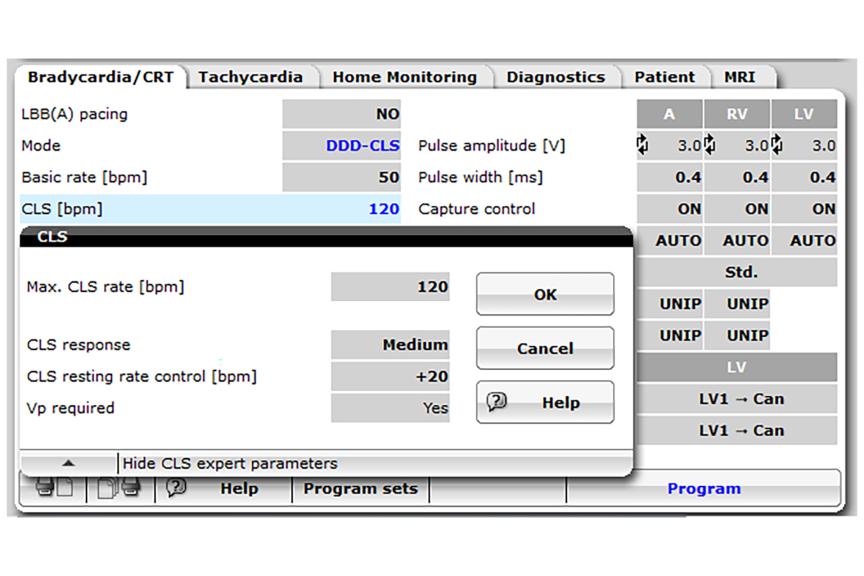
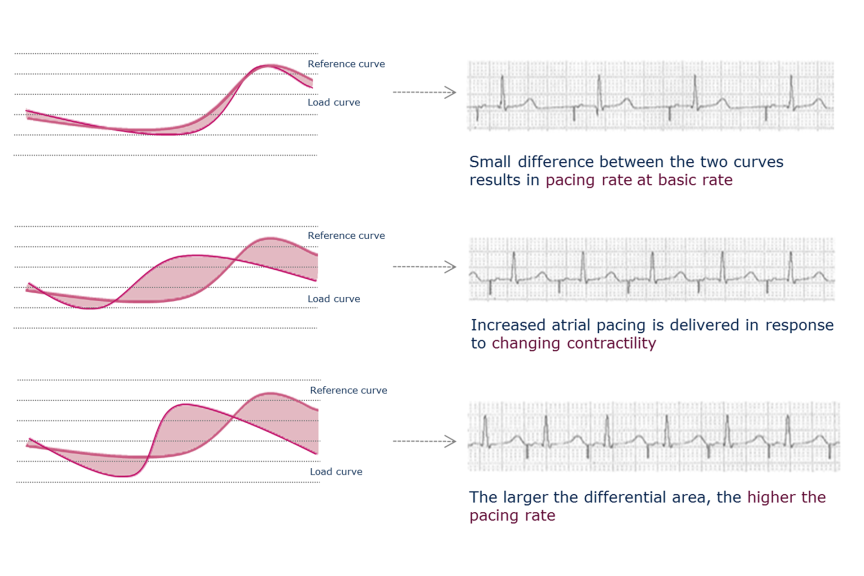
CLS can adapt to drug therapy and emotional stresses
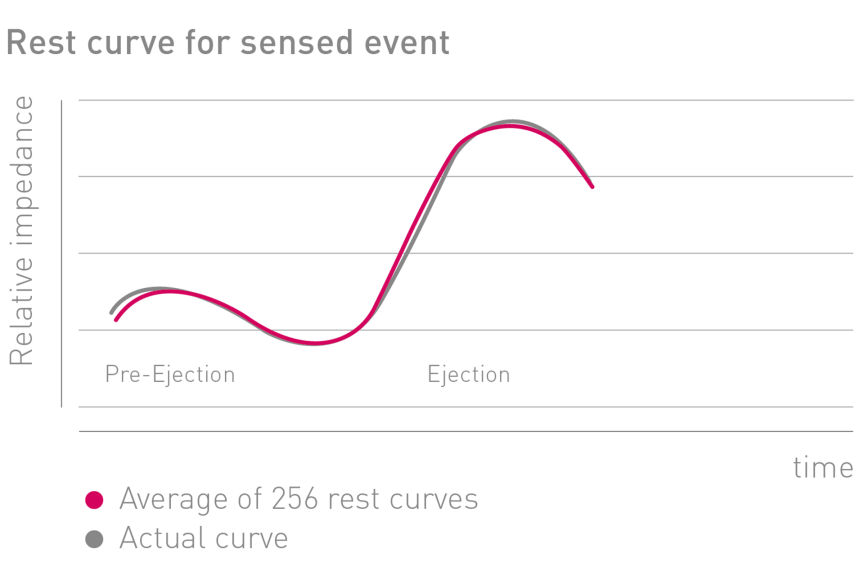
CLS can be used for patients following drug therapy. If there is ever a need to make adjustments it can be done without changing the CLS settings, as it automatically updates the curves with the new data. In the same way, according to the mental stress and the physical exercise, CLS will automatically adjust the curves with the input data and modulate the heart rate accordingly. ⁷
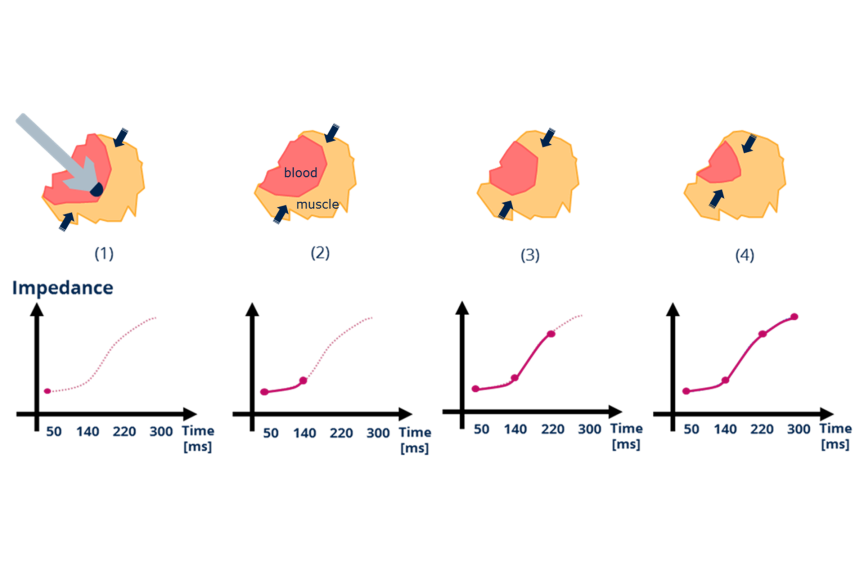
① CLS delivers gradual rate decrease based on reduction of myocardium contractility
② Only CLS provides physiological rate adaptation during mental stress
③ CLS provides rate adaptation during hemodynamic changes induced by Isoproterenol infusion
Only CLS precisely correlates between the heart rate and the blood pressure during all activities!
Learn more about CLS benefit with Dr. James Kneller here