What Causes Peripheral Arterial Disease?
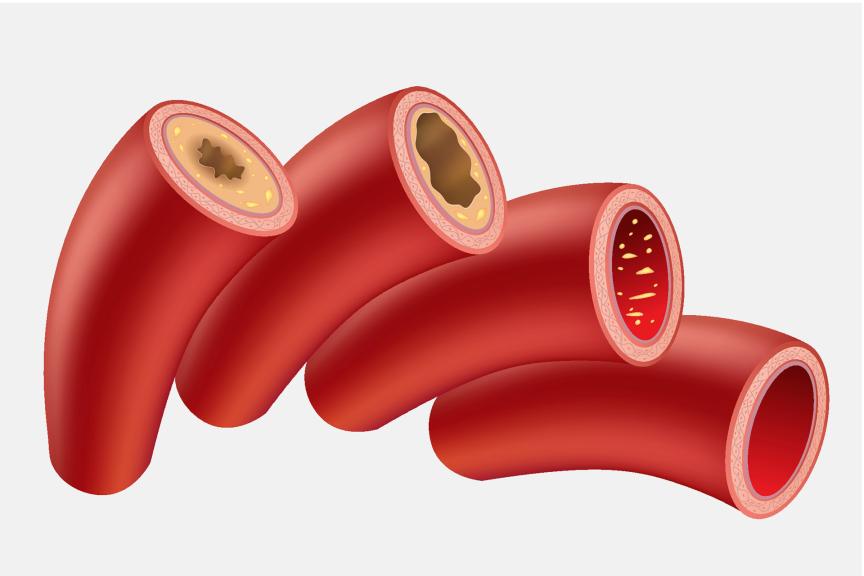
The most common cause of peripheral arterial disease is the accumulation of fatty plaque in the arteries, called arteriosclerosis. The plaque is made of cholesterol, blood fats, cellular waste, calcium and a protein called fibrin. By narrowing or blocking the arteries, the plaque reduces normal blood flow (ischemia). Without enough oxygen-rich blood, organs and tissue stop working.
The most common type of peripheral arterial disease is critical limb ischemia (CLI). CLI means that the blood flow to one or multiple limbs like your hands, legs or feet is severely blocked. 50 to 75 percent of peripheral arterial disease patients also suffer from cerebral and/or coronary arteriosclerosis, which may cause a stroke or heart attack. With cerebral arteriosclerosis, the blood vessels in the brain are affected by plaque build-up while coronary arteriosclerosis means that the blood vessels in the heart are affected by plaque build-up.
There are less common causes as well, like:
- Inflammation of blood vessels
- Arms or legs injuries
- Radiation exposure
Some of the following risk factors that increase the possibility of getting PAD can be influenced, but some cannot:
- Age (over 45 for men, over 55 for women)
- Family history of heart and vascular disease
- Diabetes
- Smoking
- Hypertension (high blood pressure)
- High levels of blood cholesterol (LDL, sometimes called “bad” cholesterol) and triglyceride levels (a type of fat found in the blood)
- Low level of "good" cholesterol (HDL)
- Excess weight or obesity
- Excessive alcohol consumption
- Excessive stress
- Not enough exercise
What Are the Symptoms of Peripheral Arterial Disease?
In the beginning, the following symptoms can indicate peripheral arterial disease:
- Tired and weak arms and legs
- Leg pain (usually in the calves)
- Arm or buttocks pain (less common)
- Burning or tingling sensation in the feet
- Numbness in the hands and feet
- Cold skin and/or changes in skin color (reddish, bluish or pale)
- Sore legs and feet, or poor wound healing
- Intermittent and severe pain while walking that subsides with rest (claudication)
- Erectile dysfunction
Symptoms including chest pain, headache, vertigo (dizziness) and sight disturbances can indicate cerebral and/or coronary circulatory disorders.

How Is Peripheral Arterial Disease Diagnosed?
Patients with risk factors should regularly undergo check-ups. The following tests are used to confirm peripheral arterial disease:
- Ankle-brachial index (ABI): a physician measures blood pressure in the ankle and in both arms. Usually, blood pressure in the ankles is the same or slightly higher than blood pressure in the arms. If the blood pressure in the ankles is significantly lower or higher than in the arms, there is strong evidence for peripheral arterial disease. If the result is unclear, measurements are repeated before and after physical activity (exercise stress test).
- Ultrasonography: an ultrasound exam that shows narrowed or blocked blood vessels and evaluates blood flow through the arteries.
- Magnetic resonance imaging (MRI): very high-quality 3D-images show vessels and existent lesions in a non-invasive exam.
- Computed tomography (CT): X-ray scans show the arteries from different angles.
- Angiography: a contrast medium is injected in the arteries before X-rays are taken. Angiography is a minimally invasive method that provides detailed information on the location and extent of arterial blockage.