Gold Standard for Two Decades: Why the Use of GoldTip is Still Unbeaten in Certain Ablation Procedures
In the midst of celebrating 60 years of service in partnership with the healthcare community, BIOTRONIK’s Electrophysiology business marked another important milestone of its own in 2023 – its 20th anniversary.
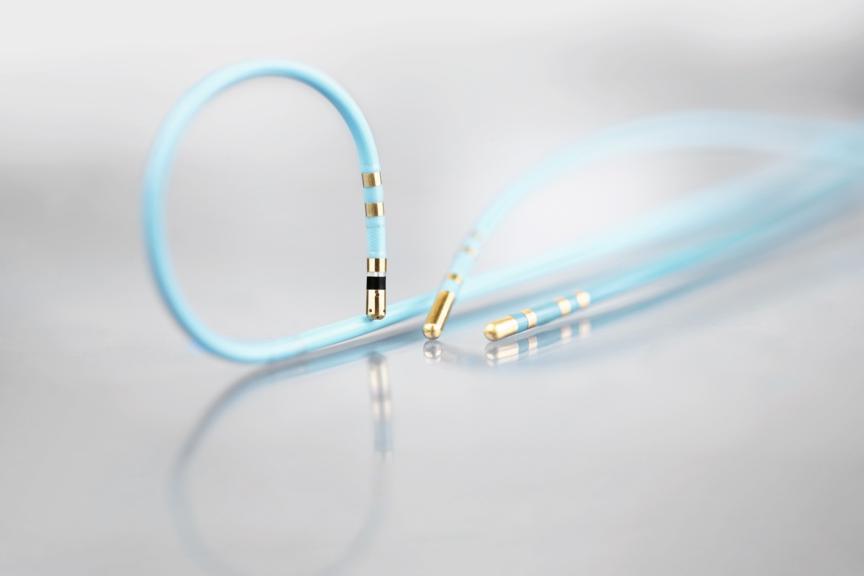
Two decades on, GoldTip ablation remains special to BIOTRONIK and has only grown in its applicability to help physicians in a variety of cases – including those with challenging anatomy.
In the second part of our two-part blog series on BIOTRONIK EP’s 20 years, we spoke with Prof. Dr. Thorsten Lewalter, Head of the Cardiology Department at the Internistisches Klinikum München Süd in Germany and one of the clinical pioneers of GoldTip ablation. He was the principal investigator of the AURUM 8 study, which provided a robust clinical basis for GoldTip ablation in the early 2000s, and one of the first practitioners to apply the technology.
We chatted with him about where the idea came from and why it’s as applicable as ever in this dynamic clinical field.
You’ve been one of the pioneers of gold use ever since its innovation. What gave you the idea to go for it?
The start of GoldTip ablation was initiated by engineers. They knew that the thermal conductivity of gold is significantly higher than platinum iridium, the conventional material in ablation catheters. So, the initial trigger came from the physics and engineering part. As physicians, we felt the need for a more powerful tool when we started ablating atrial flutter in the 90s. There was a clinical need to perform quicker and deeper lesions, but we didn’t know the best material. We worked closely with engineers who were convinced that gold is the better electrode material.
Take us through the journey you made with GoldTip from the original idea to market debut. What were the major milestones, and did anything surprise you along the way?
In vitro and in vivo, I was surprised by the visual difference of the lesions when comparing gold with platinum iridium. We organized the AURUM 8 clinical trial with nearly 20 centers Europe-wide and 450 patients. In this study, we observed different advantages of the GoldTip: Using the GoldTip enables us to deliver high output with a very small risk of charring, and the gold tip has a cooling effect. This technology allows us to follow the maximum voltage-guided approach, targeting first those thick bundles that have a high voltage presentation. All this together – gold tip, high output, maximum voltage-guided – makes the procedure very quick, very efficient, and safe.
You were the principal investigator of the AURUM 8 study. What was the result, and was it what you were expecting?
The GoldTip catheter allows us to use a 70-watt, 70 degrees target temperature – even for 50, 60, or 90 seconds – which is a very robust selection. I was surprised by the really low – nearly zero – rate of complications in terms of perforation, spasm, affecting the right coronary artery, or the AV block rate. The safety profile – even when using very robust parameters – was excellent, not only with one or two super-experienced operators but with a wide variety of operators.
During AURUM 8, your center took a different approach by going for maximum voltage. Is that still an approach you would recommend today?
The maximum voltage-guided approach was a Canadian idea. Very experienced operators like George Klein and Allan Skanes made this observation first, and I think it’s a very smart idea that conduction might not need every single tiny muscle, but it’s a mainstream concept. So, if you block the main conducting areas, the conduction will stop. This basic idea and their basic experiences demonstrated that the number of lesions to create a bidirectional isthmus block can be reduced to around 50 percent of what is needed when you perform the conventional, let’s say, point by point line concept. That’s why, I still use the maximum voltage-guided approach. We teach it to our fellows and think it is still as state-of-the-art as it ever was.
GoldTip ablation is a technology that’s now been around for quite some time. In what situation do you find it particularly useful or relevant?
The GoldTip concept is a deep lesion technology. So, everywhere we need deep lesions, transmural deep lesions, that’s the place where we use the 8-millimeter GoldTip. For atrial flutter, it’s been my standard approach for many years, and I also transform that approach to the left ventricle. We have areas where we have thick muscle structures, popular muscles, where deep lesions and catheter stability play an important role and that’s why I use it.
How has your use of GoldTip changed over time? Are you combining GoldTip and other indications?
Atrial flutter is the main area for GoldTip ablation, but in my personal daily routine, I’ve moved it to the left ventricle. I perform some of my left ventricular tachycardia ablations with a GoldTip catheter, especially in challenging areas like aortomitral continuity via a retrograde approach. There you have quite thick structures and you have a stability issue. From my perspective, this is a perfect area for the 8-millimeter GoldTip because it’s a very stable catheter and you can apply a lot of energy.
Is there anything you’d like to say about using gold in typical atrial flutter procedures, given the various innovations in EP?
We live in an amazing time. Technology is advancing very fast, and we have very sophisticated mapping concepts. I use high-density mapping in the left atrium for various reasons. But there are areas where the conventional approach is unbeaten. So, for many years, I’ve used conventional mapping and the 8-millimeter GoldTip for ablating the right atrial isthmus, and I think this is the way to go for that arrhythmia.
